5 Promising Areas in Autoimmune Research

Genetics
Autoimmune diseases often run in families, prompting researchers to delve into the genetic underpinnings of autoimmunity. One approach, referred to as a genome-wide association study or GWAS, involves analyzing hundreds or thousands of genes in large numbers of individuals to identify those that are more prevalent in disease than in health. A challenge with this approach is that there are many different gene variants in the human population. The functional effects of individual gene variants are often unknown and it may be that combinations of genes are needed to produce stronger effects that eventually predispose towards disease development. It’s essential to acknowledge the complexity of genetic effects which can include single gene changes, intricate gene combinations, and linked collections of inherited genes known as haplotypes. The HLA locus, with its association with autoimmune diseases, is a notable example of a linked collection of genes that have very prominent ties to immune responsiveness and autoimmunity. The integration of genome-wide association study data into clinical care remains a central question, crucial for categorizing patients into different treatment groups based on their genetic risks.
Environment
Shifting focus to our surroundings, autoimmunity is usually not only about genetic predisposition; exposure to the environment and pathogens plays a significant role. Millions to trillions of microorganisms colonize the human body, including bacteria, viruses, and fungi. Normally, these colonists evoke minimal inflammatory reactions, but an imbalance or wrong types of microorganisms, especially in the gut, can lead to damage. Also, location matters. Certain sites in the body are sterile and inappropriate movement of bacteria to these sites can have catastrophic effects. Mislocalization, imbalance or defective barriers can trigger inflammation, a crucial call-to-arms for the immune system to fight infections. Persistent inflammation or inappropriate immune responses can contribute to chronic disease and autoimmunity. Exploration of the link between vitamin D and autoimmune rheumatic diseases highlights the potential significance of understanding the relationship between the environment and the immune system.
Infections
 Apart from the naturally occurring microorganisms, infections are significant contributors to disease. In autoimmune conditions, individuals often experience disease flares when their immune system is stimulated by infection. Individuals with systemic autoimmunity often display what is known as a type 1 interferon signature. Type 1 interferons are a group of genes that are coordinately up-regulated in response to viral infection and are important for antiviral defense. Viral infections can also lead to immune responses, with molecules from the virus mistakenly reacting with our tissues. A prominent recent example of this “molecular mimicry” has been described with Epstein Barr virus, the virus responsible for infectious mononucleosis, and proteins in the central nervous system.
Apart from the naturally occurring microorganisms, infections are significant contributors to disease. In autoimmune conditions, individuals often experience disease flares when their immune system is stimulated by infection. Individuals with systemic autoimmunity often display what is known as a type 1 interferon signature. Type 1 interferons are a group of genes that are coordinately up-regulated in response to viral infection and are important for antiviral defense. Viral infections can also lead to immune responses, with molecules from the virus mistakenly reacting with our tissues. A prominent recent example of this “molecular mimicry” has been described with Epstein Barr virus, the virus responsible for infectious mononucleosis, and proteins in the central nervous system.
The COVID-19 context adds a layer of complexity. Individuals with severe infections produce various autoantibodies and antibodies against immune system signaling molecules known as cytokines. This prompts questions about the immune system’s behavior during severe illness and its potential contribution to chronic autoimmune diseases. Long COVID is also under scrutiny, exploring whether persistent symptoms signify a loss of self-tolerance. These areas remain active in research, unraveling the mysteries of the immune system’s behavior in diverse health conditions.
Biomarkers of Disease Susceptibility and Established Disease
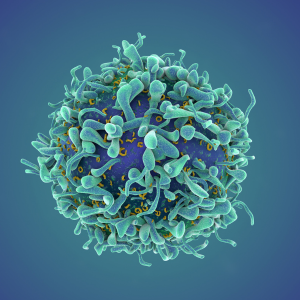
 An active area of study involves early biomarkers of disease, with antibodies being prominent examples. Autoantibodies, crucial for diagnosing autoimmune diseases, may be present before an official diagnosis, indicating their potential role in disease development. Researchers are also exploring immune cells (such as B cells and T cells) as biomarkers, analyzing thousands to millions of their receptors through massively parallel sequencing techniques. Applying AI and machine learning to these massive datasets holds promise for future biomarker discovery because some of these cells may precede antibody formation and could be used for immune monitoring.
An active area of study involves early biomarkers of disease, with antibodies being prominent examples. Autoantibodies, crucial for diagnosing autoimmune diseases, may be present before an official diagnosis, indicating their potential role in disease development. Researchers are also exploring immune cells (such as B cells and T cells) as biomarkers, analyzing thousands to millions of their receptors through massively parallel sequencing techniques. Applying AI and machine learning to these massive datasets holds promise for future biomarker discovery because some of these cells may precede antibody formation and could be used for immune monitoring.
Defining established diseases poses challenges due to diverse components, such as dysregulated immune systems and abnormal responses to self. Traditional medical definitions often overlook psychosocial impacts, financial burdens, and quality of life aspects, highlighting the need for comprehensive long-term studies.
Targeted Therapies
A significant focus lies in understanding immune changes in autoimmune diseases. Traditional therapies target specific molecules, tailored for each patient to maximize benefits and minimize harmful side effects. However, the variability in treatment efficacy within and across diseases remains a challenge.
In addition to therapeutic antibodies and small molecule inhibitors, there are cell-based approaches that are being explored for the treatment of autoimmune diseases. T cells with genetically engineered receptors that bypass the requirement for HLA recognition, known as chimeric antigen receptor or CAR-T cells are being tried in patients with severe refractory disease. Creating CAR T-cells expressing autoantigens recognized by the patient’s immune system presents a potential breakthrough, for diseases with well-established autoantigens like pemphigus vulgaris.
Protecting tissues from autoimmune attacks is also a focus. Normally the body has an extensive “clean-up” system that removes dying and injured cells without promoting inflammation. When there are defects in this system or alterations in the tissues that lead to inappropriate immune recognition, tissue damage can ensue. There is a need to unravel the mechanisms behind disease chronicity and reverse chronic inflammation. Early treatment with immunomodulatory therapies is crucial, particularly for diseases like type 1 diabetes, where early immune intervention may prolong or ultimately prevent tissue damage.
For those with established diseases, the primary goal is to induce quiescence, drawing inspiration from cancer therapeutics. The aim is to achieve long-term remissions with short exposures to optimized medicines, considering individual genetics and disease type.
Once remission is achieved, maintenance of self-tolerance may involve low-dose, specific, and safe therapies, with advanced immune assays to monitor disease reemergence. Managing disease is crucial for patients, involving strategies to handle flares, limit organ damage, and improve overall quality of life. In summary, a nuanced approach is essential, identifying at-risk individuals and intervening early, minimizing damage during disease initiation, limiting organ damage during acute disease, and ultimately inducing long-term remission and, in some cases, cures.
Looking Ahead
 Autoimmune research is buzzing with excitement and promise as scientists explore new ways to understand, prevent, and treat autoimmune conditions. Researchers are working towards precision medicine approaches for autoimmune disease, not unlike what is currently being offered to patients with cancer: administering the right therapy to the right patient at the right time, maximizing therapeutic benefits. This integrative approach holds a lot of promise for the future, bringing hope for better treatments and, ultimately, delivering cures. The future is bright, and the autoimmune community can look forward to significant advancements in these areas of biomedical research.
Autoimmune research is buzzing with excitement and promise as scientists explore new ways to understand, prevent, and treat autoimmune conditions. Researchers are working towards precision medicine approaches for autoimmune disease, not unlike what is currently being offered to patients with cancer: administering the right therapy to the right patient at the right time, maximizing therapeutic benefits. This integrative approach holds a lot of promise for the future, bringing hope for better treatments and, ultimately, delivering cures. The future is bright, and the autoimmune community can look forward to significant advancements in these areas of biomedical research.
Join our email list
Receive the latest blog articles, news, and more right to your inbox!
Related articles you might be interested in

Autoimmune Association Announces Inaugural Hope Journey Walk Inviting Communities to “Lace Up for Hope”

Study Reveals Top Environmental Concerns Impacting Autoimmune Patients

Meet the 2025 Young Adult Advisory Council: Empowering the Next Generation of Autoimmune Advocates

Advocates Take Action at the Autoimmune Association’s Legislative Fly-In
Find more resources on autoimmunity
Learn more about autoimmunity, diagnosis tips, how to find a physician, and more.